What is Diabetes
Diabetes is a metabolic disorder that occurs when the pancreas is no longer able to make insulin, or when the body cannot make good use of the insulin it produces. Insulin is a hormone made by the pancreas (an organ of body responsible for insulin production), that acts like a key to let glucose from the food we eat pass from the blood stream into the cells in the body to produce energy. All carbohydrate foods are broken down into glucose in the blood. Insulin helps glucose get into the cells.
not being able to produce insulin or use it effectively leads to raised glucose levels in the blood (known as hyperglycaemia). Over the long-term high blood glucose levels are associated with damage to the body and failure of various organs.
Symptoms
In type 1 diabetes, symptoms are often sudden and can be life-threatening; therefore it is usually diagnosed quite quickly. In type 2 diabetes, many people have no symptoms at all, while other signs can go unnoticed being seen as part of getting older.
Therefore, by the time symptoms are noticed, complications of diabetes may already be present.
Common symptoms include:
• Being more thirsty than usual
• Passing more urine
• Feeling tired and lethargic
• Always feeling hungry
• Having cuts that heal slowly
• Itching, skin infections
• Blurred vision
• Unexplained weight loss
• Headaches
• Feeling dizzy
• Leg cramps
Types of Diabetes
There are three main types of diabetes:
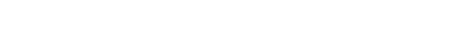
Type 1 diabetes used to be called juvenile-onset diabetes. It is usually caused by an auto-immune reaction where the own body’s defence system attacks the cells that produce insulin. The reason this occurs is not fully understood. People with type 1 diabetes produce very little or no insulin. The disease may affect people of any age, but usually develops in children or young adults. People with this form of diabetes need insulin every day in order to control the levels of glucose in their blood. If people with type 1 diabetes do not have access to insulin, they can develop complications associated with diabetes.
Type 2 diabetes used to be called non-insulin dependent diabetes or adult-onset diabetes, and accounts for at least 90% of all cases of diabetes. It is characterised by insulin resistance and relative insulin deficiency, either or both of which may be present at the time diabetes is diagnosed. The diagnosis of type 2 diabetes can occur at any age. Type 2 diabetes may remain undetected for many years and the diagnosis is often made when a complication appears or a routine blood or urine glucose test is done. It is often, but not always, associated with overweight or obesity, which itself can cause insulin resistance and lead to high blood glucose levels. People with type 2 diabetes can often initially manage their condition through exercise and diet. However, over time most people will require oral drugs and or insulin.
Both type 1 and type 2 diabetes needs proper treatment . There is no such thing as mild diabetes.
Gestational diabetes (GDM) is a form of diabetes consisting of high blood glucose levels during pregnancy. It develops in one in 25 pregnancies worldwide and is associated with complications to both mother and baby. GDM usually disappears after pregnancy but women with GDM and their children are at an increased risk of developing type 2 diabetes later in life. Approximately half of women with a history of GDM go on to develop type 2 diabetes within five to ten years after delivery.
Other specific types of diabetes also exist.
Diagnosis
To be diagnosed with diabetes, you must meet one of the following criteria:
• Have symptoms of diabetes (increased thirst, increased urination, and unexplained weight loss) and a blood glucose level equal to or greater than 200 milligrams per deciliter (mg/dL). The blood glucose test is done at any time, without regard for when you last ate (random plasma glucose test or random blood sugar test).
• Have a fasting blood glucose level that is equal to or greater than 126 mg/dL. A fasting blood glucose test (fasting plasma glucose) is done after not eating or drinking anything but water for 8 hours.
• Have a 2-hour oral glucose tolerance test (OGTT) result that is equal to or greater than 200 mg/dL. An OGTT is most commonly done to check for diabetes that occurs with pregnancy (gestational diabetes).
• Have a hemoglobin A1c that is 6.5% or higher.
Your doctor may repeat the test to confirm the diagnosis of diabetes.
If the results of your fasting blood glucose test are between 100 mg/dL and 125 mg/dL, your OGTT result is between 140 to 199 mg/dL (2 hours after the beginning of the test), or your hemoglobin A1c is 5.7% to 6.4%, you have prediabetes. This means that your blood glucose is above normal but not high enough to be diabetes. Discuss with your doctor how often you need to be tested.
Insulin
What is insulin?
Insulin is a hormone produced by our pancreas that regulates the level of glucose (commonly called as glucose ) in the blood. Our body requires a steady amount of glucose throughout the day and that glucose comes from the food we eat. Insulin makes our body’s cells absorb glucose from the blood and convert it into energy. When there is very little insulin in the blood or none at all, glucose is not absorbed by most body cells and our body will not be able to function properly which leads to Hyperglycaemia (high blood glucose).
Why do I need Insulin?
We all need energy to grow and live life. We get energy from the food we eat. The food we eat is broken down into glucose. Glucose needs to enter the cells in your body before it can be used as energy. If the glucose cannot enter the cells, you will get tired. Insulin opens the doors to the cells in your body, so that glucose can enter the cells and be used. If insulin will not be there , there will be increased glucose levels in blood which can lead to some complications associated with diabetes like Nephropathy (kidney problem), Retinopathy (Eye problem), Neuropathy and cardiac problems.
How does the normal body produce and use insulin
In a healthy person there are following two stages of insulin secretion by the pancreas:
Basal insulin secretion:This is the secretion of insulin that happens to regulate glucose level throughtout the day. During fasting stage( when we haven’t eaten food) liver produce stored glucose( excess glucose from the food we eat gets stored in the liver) into the blood that is absorbed by the cells to generate energy. If basal insulin secretion in not there the glucose levels will rise in our blood and this will result in uncontrolled Fasting Blood Glucose.
Post meal insulin secretion: When we eat food(breakfast,lunch,dinner,snacks),the glucose levels start rising in our blood. To regulate this sharp increase in the glucose levels the pancreas secrete insulin proportional to the food we eat. In diabetes enough insulin is not secreted by our pancreas and there will be high glucose levels in our blood after we eat food. This results in uncontrolled postprandial blood glucose( commonly called as PP glucose).
Types of Insulin
There are three main parameters in insulin action and they are onset, peak and duration of Insulin action.
Your doctor will work out with you and decide what type of insulin is right for you.
The main types of Insulin are
• Fast/rapid-acting insulin is clear in appearance, and starts to work from 5 to 20 minutes. It peaks approximately 1 hour later, and lasts from 3 to 5 hours. You must eat immediately within 10 minutes after injecting fast-acting insulin. For example, Insulin Lispro, Aspart, Apidra.
• Short-acting insulin is clear in appearance. It begins to work within half an hour, so you need to inject half an hour before eating, and it peaks at 2 to 4 hours and last for 6 to 8 hours. For example Insulin R(Regular)
• Intermediate-acting insulin is cloudy in appearance. It begins to work about 1 and a half hours after injecting, peaks at 4 to 12 hours and lasts for 16 to 18 hours. Before injecting, check the leaflet included in the pack for instructions on preparing the insulin. For example Insulin NPH
• Premixed insulin is cloudy in appearance and contains pre-mixed combinations of either a fast-acting or a short-acting insulin and an intermediate-acting insulin. This makes injecting easier by giving two types of insulin in one injection. This insulin can be taken before a meal to provide a stable level of insulin for some time after the meal. Before injecting, check the leaflet included in the pack for instructions on preparing the insulin. For example Insulin 30/70, Insulin Mix 25/75,Insulin 50/50
• Long-acting insulin is clear in appearance. It is also called basal insulin. It typically has no pronounced peak and lasts for up to 24 hours.For example Insulin Glargine.
Storage and handling of Insulin
• Check the expiration date before using, and don’t use any insulin beyond its expiration date.
• Never store insulin in the freezer, direct sunlight, or in the glove compartment of a car.
• Inspect your insulin before each use. Look for changes in color or clarity. Look for clumps, solid white particles or crystals in the bottle or pen. Insulin that is clear should always be clear and never look cloudy.
• Always store unopened vial/catridges in refrigerator at 2-8 degree temperature.
• Once in use insulin pen should be kept at below 30 degree temperature.
• While travelling you can use ice pack or insulated box.
• Avoid extremes of cold or heat. Temperatures can alter the effectiveness of the insulin.
Important points to remember while giving the insulin and travelling
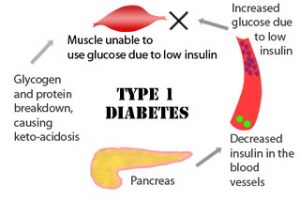
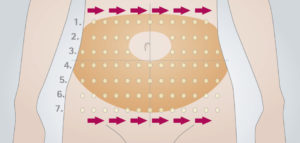
• Insulin is absorbed fastest when injected into the subcutaneous tissue in the abdomen (stomach), and somewhat
less quickly in the upper arms, thighs, and buttocks/hips.
• No need to apply alcohol swab at the site of injection if you are taking bath regularly
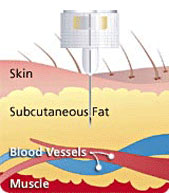
• Insulin should be given in subcutaneous fat.
• An insulin cartridge of 3 ml (100 IU/ml) contains 300 units of insulin.
• An insulin vial of 10 ml (40 IU/ml) contains 400 units.
• Always use 40 IU syringe with 40 IU Insulin vial.
• Always use 100 IU syringe with 100 IU insulin vial.
• Insulin site rotation is required for proper function of insulin.
• Always check your insulin sites for preventing the Lipoatrophy.
• Avoid vigorous shaking of insulin.
• Carry insulin in ice packs while travelling and protect insulin from light,heat and extreme cold temperature.
Don’t use if
• Clear insulin has turned cloudy or changed colour
• The expiry date has been reached
• Insulin has been frozen or exposed to high temperatures
• Lumps,flakes or frozen crystals seen in catridge/vial.
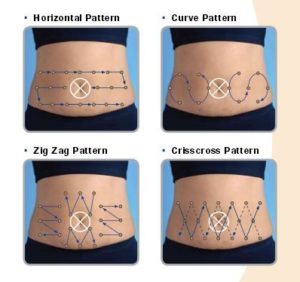
Rotating injection site
Site rotation is an important component of insulin therapy, especially for people with diabetes who inject three or more times a day. Proper site rotation may result in more consistent insulin absorption and minimize development of lipohypertrophy/lipodystrophy.Injection into lipodystrophied sites, results in an erratic absorption of the drug, leading to glycaemic variability making it difficult to achieve suitable metabolic control.Annual examination of injection site is recommended for evidence of lipodystrophy.

What is lipohypertrophy?
Lipohypertrophy is an abnormal accumulation of fat underneath the surface of the skin. It’s most commonly seen in people with type 1 diabetes. In fact, up to 50 percent of people with type 1 diabetes experience it at some point.Repeated insulin injections in the same location can cause fat and scar tissue to accumulate.
Symptoms of lipohypertrophy
The main symptom of lipohypertrophy is the development of raised areas under the skin. These areas may have the following characteristics:
- small and hard or large and rubbery patches
- surface area over 1 inch in diameter
- a firmer feel than elsewhere on the body
Areas of lipohypertrophy can cause delays in absorption of medication administered to the affected area, like insulin, which can result in difficulties controlling blood sugar.
Lipohypertrophy areas should not:
- be hot or warm to the touch
- have redness or unusual bruising
- be noticeably painful
These are all symptoms of a potential infection or injury. See a doctor as soon as possible if you have any of these symptoms. Lipohypertrophy is not the same as when an injection hits a vein, which is a temporary and one-time situation and has symptoms that include bleeding and a raised area that may be bruised for a few days.
Treating lipohypertrophy
It’s common for lipohypertrophy to go away on its own if you avoid injecting in the area. In time, the bumps may get smaller. Avoiding the injection site is one of the most important parts of treatment for most people. It can take anywhere from weeks to months (and sometimes up to a year) before you may see any improvement.
Causes of lipohypertrophy
The most common cause of lipohypertrophy is receiving multiple injections in the same area of skin over an extended period of time. This is mostly associated with conditions like type 1 diabetes which require multiple injections of medication on a daily basis.
Risk factors
There are several factors that increase the odds of developing lipohypertrophy. The first is receiving injections at the same location too often, which can be avoided by consistently rotating your injection sites. Using a rotation calendar can help you keep track of this.Another risk factor is reusing the same needle more than once. Needles are meant to be single-use only and are dulled after each use. The more you reuse your needles, the greater your chance of developing this condition.Poor glycemic control, duration of diabetes, needle length, and duration of insulin therapy are also risk factors.
Preventing lipohypertrophy
Tips for preventing lipohypertrophy include:
- Rotate your injection site each time you inject.
- Keep track of your injection locations (you can use a chart).
- Use a fresh needle each time or avoid using is more than four times.
- When injecting near a previous site, leave about an inch of space in between the two.
Also, keep in mind that insulin absorbs at different rates depending on where you inject.In general, your abdomen absorbs injected insulin the fastest. After that, your arm absorbs it most quickly. The thigh is the third fastest area for absorption, and the buttocks absorb insulin at the slowest rate.
Make it a habit to routinely inspect your injection sites for signs of lipohypertrophy. Early on, you may not see the bumps, but you’ll be able to feel the firmness under your skin. You may also notice that the area is less sensitive and you feel less pain when you inject.
Sick day guidelines
The blood sugars usually increase when you are sick. With proper planning, the risks from illnesses are not much greater than for anyone else. Sick days include illnesses like colds and flu. They also include times like dental work and surgery when your body will be under stress and you may not be eating or drinking normally. When you have type 1 diabetes, everyday illnesses or infection can cause both high and low blood glucose levels. It’s important to be prepared before you get sick – have a personalized sick day action plan and sick day management kit ready to use at the earliest sign of illness. Discuss putting together your sick day action plan and kit with your diabetes team.
What is a sick day?
A sick day is when you have an illness or infection and need to make changes to your usual diabetes management to keep blood glucose levels in the target range. These changes are usually only needed until you are well again.
Why it’s important to manage sick days
When you have type 1 diabetes and you are unwell, high blood glucose levels increase your risk of developing ketones. This can lead to diabetic ketoacidosis, which can be life-threatening.
What are ketones?
When there is not enough insulin in the body, glucose can’t enter the body’s cells to provide energy. Instead, the body breaks down fat as an alternative source of energy. This breakdown of fat produces ketones, which are toxic to the body in large amounts.
What is diabetic ketoacidosis?
Diabetic ketoacidosis (DKA) is a serious condition that occurs when the levels of glucose and ketones in the blood are too high. The blood becomes too acidic because of a build-up of ketones, and there is loss of body salts and fluids. If you have large amounts of ketones in your blood or urine, this suggests that you may have DKA and you need urgent medical attention.
Signs of DKA can include:
• nausea, vomiting and/or stomach pain
• rapid breathing or breathlessness » drowsiness, confusion or weakness
• increased thirst or dry mouth
• reduced or no urine output breath that smells fruity.
General guidelines for sick day management
o Drink plenty of fluids. Vomiting, diarrhea and fever cause you to loose fluids and you need to replace them to
prevent dehydration.
o Drink small sips of liquid often, rather than a large amount all at once.
o Drink at least 250 -300 ml of fluid every hour while awake or every 30 minutes or so,
o If you are eating your normal food, the extra fluids should be sugar-free.
o If you can’t eat, take your food in liquid form.
o If vomiting, avoid solid foods until vomiting has stopped.
o Do not stop taking your insulin.
o Insulin is needed when you are sick, even if you are not eating. Never skip an insulin dose entirely.
o The insulin dose may need to be adjusted on sick days. If you are unsure of how much insulin to take, consult your physician/medical team.
o Check your blood glucose and ketones often
Seek urgent medical attention if you have any of these symptoms.
• Feeling drowsy or confused
• have deep, rapid breathing or shortness of breath
• have stomach pain
• have a ‘fruity’ odour to your breath (a sign of DKA)
• can’t keep food or fluids down and are experiencing persistent vomiting or diarrhoea
This is a serious medical emergency and can be life threatening if not treated properly. If these symptoms are present, contact your doctor or go to hospital immediately.
Hypoglycemia
Hypoglycemia, sometimes called a hypo or low, is a condition that occurs when a person’s blood glucose level (BGL) has dropped too low, below 70 mg/dl . It is important to treat a hypo quickly to stop the BGL from falling even lower and the person becoming seriously unwell.
Hypoglycemia can make it hard to concentrate and carry out everyday activities. Some activities, such as driving and operating machinery, are not safe if BGLs are less than 80 mg/dl.
Hypoglycemia only occurs in people who take insulin or certain other glucose lowering tablets. People who manage their diabetes with healthy eating and physical activity are not at risk of a hypo.
Causes of hypoglycemia
Hypoglycemia can be caused by one or a number of events, such as:
• Too much insulin or other glucose lowering diabetes tablets
• Delaying or missing a meal
• Not eating enough carbohydrate
• Unplanned physical activity*
• More strenuous exercise than usual*
• Drinking alcohol – the risk of hypoglycemia increases, the more alcohol you drink
*Hypoglycemia may be delayed for 12 hours or more after exercise
Symptoms
Symptoms of hypoglycemia vary from person to person. Early signs and symptoms may include:
• Trembling or weakness
• Sweating
• Paleness
• Hunger
• Light headedness
• Headache
• Dizziness
• Pins and needles around mouth
• Mood change
If the BGL continues to drop, more serious signs and symptoms may occur.
Later signs and symptoms of hypoglycemia may include:
• Lack of concentration/ behaviour change
• Confusion
• Slurred speech
• Not able to treat own hypo
• Not able to drink or swallow
• Not able to follow instructions
• Loss of consciousness
• Fits/seizures
Hypoglycemia can be classified as mild or severe. A mild hypo occurs when a person can treat their own hypo. A severe hypo occurs when a person needs help from someone else to treat their hypo.
Treating hypoglycemia
What should I do if I suspect I am having hypoglycemia?
When hypoglycemia is suspected, testing blood glucose is the best way to confirm the symptoms. If testing is not possible, or testing confirms low glucose, one of these quick-fix foods should be consumed right away to raise blood glucose:
• 1/2 cup of any fruit juice.
• The amount equal to 15 grams of carbohydrate.
• Glucon D power.
• 1/2 cup of a regular-not diet-soft drink.
• 1 cup of milk with sugar
• 2 or 3 pieces of hard candy
• 1 tablespoon of sugar or honey
• 1/2 can of regular soft drink (not ‘diet’) OR
• 1/2 glass of fruit juice OR
• 3 teaspoons of sugar or honey OR Glucose tablets equivalent to 15 grams carbohydrate.
After you treat the initial symptoms, wait 20 minutes and test your blood again. If your blood glucose level is still low or you still feeling symptoms, repeat the above treatment. Also, be sure to write down that you had Hypoglycemia.
• Having no symptoms of low blood glucose at all is a dangerous situation! If you have a blood sugar reading below 70 mg/dl and aren’t experiencing any of the symptoms described above, you should immediately treat your low blood sugar level. Even if you are feeling fine, this situation still needs to be treated. Make sure to notify your doctor of this event.
What happens if I don’t treat hypoglycemia?
If not treated quickly, the BGL can continue to drop, which may result in the brain not getting enough glucose. This can cause unconsciousness or fits/seizure.
What to do if the person is unconscious, drowsy or unable to swallow
If a person with diabetes is unconscious, drowsy or unable to swallow then it is an emergency.
Do not give them any food or drink by mouth, treat as follows:
1. Place them on their side making sure their airway is clear
2. Give an injection of Glucagon if available and you are trained to give it
3. Phone for an ambulance stating the person is unconscious AND that the person has diabetes
What is glucagon?
Glucagon is a hormone which raises the BGL. It is injected into a muscle to reverse severe hypoglycemia in people with diabetes. If you are able to treat your own ‘hypo’, you do not need Glucagon which is always given by another person. Your doctor will recommend you have Glucagon on hand in case of a severe ‘hypo’ and will show you, your family and friends how to use it.
Impaired Awareness of Hypoglycemia (IAH)
Impaired Awareness of Hypoglycemia (IAH) occurs when people do not feel the early warning symptoms of hypoglycemia and only realise they are hypo when their BGLs drop very low or when they check their BGL. If you have had diabetes and hypos for many years the risk of not feeling the symptoms of hypos is more common. IAH can be dangerous because by the time you realise you are having a hypo you may find it hard to treat it and you could become unconscious.
If you have ‘hypos’ without symptoms or your symptoms change, you may need to check your blood glucose more often. Always treat BGLs at 70mg/dl or below, even if you feel fine. If you have low BGLs without any symptoms you need to discuss this with your doctor .
Precautions to prevent hypoglycemia
• Don’t skip meals or snacks.
• Eat your meals on time and always carry fast acting carbohydrates with you.
• Make a note of any ‘hypos’ you have and discuss it with your doctor
• Learn to adjust your food and insulin with exercise.
• Test your blood sugar on schedule and write it on log book.
• Do extra tests when you don’t feel normal, and write down the results in your log book.
• Learn your body’s warning signs of hypoglycemia so that you can treat it quickly.
• When you notice symptoms, test your blood sugar if you can.
• If your blood sugar is low or if you cannot test, treat yourself for low blood sugar. If your next meal is more than an hour away, have a snack.
• Always wear or carry diabetes identification.
• Educate family members, friends, or coworkers on symptoms of and treatment for low blood sugar.
• Be sure to keep foods that contain sugar or glucose products with you at all times.
• Be sure to write insulin dosage if hypoglycemia occurs.
• Look for the cause of your ‘hypo’ so you can try to prevent it from occurring again.
Checklist for uncontrolled blood glucose
Patient related factors
• Insulin/ meal related mistake
• Poor diet control
• Wrong insulin technique/ development of Lipohypertrophy
• Poor insulin storage
Drug related factors
• Tempered insulin
• Inadequate dose of insulin
• Insulin potency
Other factors
• Lifestyle adjustments
• Stress